As a sports medicine physician, I talk to patients every day about imaging—when to get it, what type of imaging to expect, and whether it’s even necessary. I have at least a few patients each day requesting me to order MRIs of specific joints or body parts. Many people believe that more imaging leads to better care. After all, the more information we have, the better, right?
One of the most important principles I was taught in medical school still holds true: Before ordering any test, ask yourself—will the result change how I treat the patient? If the answer is no, then that test might not be helpful.
For example, if a patient comes in with low back pain, there could be several possible causes (as you already know from my low back pain article!). The pain could be from discs, nerves, bones, or soft tissue (muscle or ligament). While the most common cause is muscular or soft tissue, this type of pain generally does not need imaging and in fact, these structures often look normal on imaging; But if we order an MRI, we will almost certainly see disc degeneration, narrowing of the spaces for the nerves, and wear and tear consistent with arthritis.
Understandably, all these words sound scary for patients, but in reality, these findings are usually not clinically relevant findings and are just part of normal aging. In an ideal world, the physician who ordered the test should be performing a detailed physical exam and counseling the patient on what is and what is not relevant from the imaging. Unfortunately, this does not always happen and the patient is often led down a path of more tests, invasive injections, and unnecessary workup. In some cases, it can even lead patients to have surgical consultations and surgeries, even if the findings are not related to their symptoms and pain. Basically, what gets treated are the imaging findings and not the patients themselves.
Now let’s see how concepts relate to the idea of scanning your whole body.
The New Trend: Full Body MRIs for Cancer Screening
In recent years, a new trend has emerged: full body MRI scans marketed as preventive health tools, often targeting people who are asymptomatic and just want to “check for cancer.” These scans are sometimes advertised as a way to “get ahead” of disease and feel more in control of your health.
This has understandably caught people’s attention, especially following social media posts from wellness influencers and high profile celebrities who underwent them. Cancer is scary, and the idea of catching it early—even before it causes symptoms—sounds like a no-brainer (cost aside). But the reality of full body MRI screening is more complex.
Below, I will discuss what a full body MRI is, what it can (and cannot) detect, what the data suggests, and my own take on how to approach them.
What Is an MRI, and How Is It Used in Screening?
MRI (magnetic resonance imaging) is a non-invasive test that uses a strong magnetic field and radio waves to create detailed images of soft tissues inside your body—muscles, organs, blood vessels, brain, spinal cord, etc. It does not use ionizing radiation, unlike CT scans or X-rays, which is a plus in terms of safety.
In cancer screening, full body MRIs aim to scan multiple organs and systems at once to look for signs of tumors or other abnormalities. Some private companies now offer this as part of “executive physicals” or high-end wellness packages, sometimes bundled with genetic testing, blood work, or AI-based imaging analysis.
The Pros and Cons Full Body MRI Screening
Potential Benefits:
Radiation-free: Unlike CT scans, MRI does not expose you to any ionizing radiation, making it safe for repeated use.
Early detection: In some cases, an MRI might catch tumors in places like the kidneys, brain, breast, liver, or other soft tissues before they cause symptoms or show up on other tests, such as routine bloodwork.
Incidental findings that actually matter: Occasionally, a full body MRI might uncover a significant condition—such as an aortic or brain aneurysm (a potentially dangerous blood vessel abnormality)—that wasn’t previously known and needs follow-up.
But there are some important downsides:
1. Not All Cancers Show Up on MRI
MRI is not the best tool for detecting many common cancers. For example:
Lung cancer is much better seen with a low-dose CT scan, especially for small nodules (<5-6mm).
Colon cancer is most effectively screened with a colonoscopy. MRI would only detect tumors if they are large enough to cause structural changes or spread
Prostate cancer typically requires a targeted prostate MRI or biopsy based on blood test results.
Ovarian and Uterine Cancers are better seen on ultrasound or targeted pelvic MRI, especially small tumors.
Esophageal and Stomach Cancers are better seen by endoscopy (internal camera) with biopsy.
Bladder cancer is better seen with cystoscopy (internal camera)
Leukemia and Lymphomas may be missed if they are early or non-mass-forming lymphomas. Blood tests and bone marrow biopsies may be required.
Skin Cancers could only be detected on MRI if they were metastatic. Otherwise, superficial skin lesions should be evaluated by skin exams.
As you can see, a “normal” full body MRI does not necessarily mean you are cancer-free.
2. False Positives Are Common
This is my biggest concern with full body MRI as a screening tool. In general, MRI is very sensitive. As you’ve seen in my examples above, it often picks up incidental findings—cysts, benign nodules, mild degenerative changes, or other harmless abnormalities. While these might look concerning on a scan, they often turn out to be clinically irrelevant. Still, once something abnormal is found, it typically triggers more testing: follow-up MRIs, CT scans, blood tests, biopsies, or even surgeries.
This cascade of unnecessary workup can lead to:
Iatrogenic harm — meaning harm we unintentionally cause, such as complications from invasive tests
Radiation exposure — from follow-up imaging, like CT scans, which involve ionizing radiation
Stress and anxiety — over “maybe” diagnoses
3. Low Predictive Value in Healthy Populations
Predictive value is an important idea to understand when you're looking at any type of test result. It basically answers two questions:
If my test comes back positive (or abnormal), how likely is it that I actually have the disease?
If it’s negative (or normal), how confident can I be that I don’t have the disease?
It’s not just about whether the test says “yes” or “no” — it’s about how much you can trust that answer based on your situation.
In this context, even if an MRI scan finds something “suspicious,” the chance that it actually represents a serious or life-threatening disease is very low in asymptomatic people. This is what we mean by a low positive predictive value—lots of “red flags” that turn out to be nothing.
A 2020 review looking at multiple studies totaling over 6000 whole body MRI participants found that 95% of subjects had at least one “abnormal” finding (this included minor findings). More importantly though, 30% of the subjects had findings concerning enough to warrant additional testing. However, in total, after the additional workup, <2% ended up being “suspicious” for cancer and ultimately 1.1% were confirmed to have cancer. This is a very low yield test – even when patients tested “positive” for possible cancer, almost none of them actually had cancer.
It is important to mention here that if you have a strong family history of cancer or genetic mutations, the positive predictive value would be higher. For example, a 2017 study in JAMA found that for those specifically with Li-Fraumeni syndrome (a very rare genetic disorder), the positive predictive value for full body MRIs was closer to 50%. While still only half of the suspicious test results ultimately turned out to be cancer, this represents a much higher detection rate compared to screenings in the average asymptomatic person.
4. Financial Cost
Currently, the cost can vary from $1500 to $3000 per scan, depending how comprehensive it is and what body parts you want included, although it is possible over the next 3-5 years the cost may come down as technology improves and AI analysis in radiology becomes integrated more broadly. But keep in mind - this is just the cost of scan alone, not the cost of the extra tests and interventions that may come from it.
What are medical organizations saying?
Most medical organizations are aligned in their recommendation against full body imaging for screening:
The American College of Radiology (ACR) issued a statement in April 2023 that it “does not believe there is sufficient evidence to justify recommending total-body screening for patients…In addition, the ACR is concerned that such procedures will lead to the identification of numerous non-specific findings that will not ultimately improve patients' health but will result in unnecessary follow-up testing and procedures, as well as significant expense.”
The American Academy of Family Practice similarly states: “There are no data suggesting that these (Whole-body) imaging studies will improve survival or improve the likelihood of finding a tumor (estimated tumor detection is less than 2% in asymptomatic patients screened).”
The American College of Preventive Medicine (ACPM) also does not recommend whole-body MRI scans for early tumor detection in asymptomatic patients.
Bringing it Back to Sports Medicine: Incidental Arthritis
Let’s return to my back pain patients. When the scan comes back showing arthritis or disc degeneration, common and expected findings as we age, patients often panic and some start believing they need surgery or worry they’re deteriorating, even when they are functional and this is not the cause of their pain. Even if their pain is muscular, they may not accept that these findings are irrelevant, and understandably, they feel the need to “fix” the problem.
I have had several patients who go on to see surgeons as they’re convinced they need surgery. The surgeon often ends up operating (remember that the best surgeons know when not to operate). Postoperatively, they have gone on to be diagnosed with “failed back surgery syndrome” or chronic pain. This is an unfortunate situation because it’s not that they “failed” back surgery – they should have never had back surgery to begin with! And this series of events was triggered by the initial unnecessary MRI.
Now imagine these same reactions across the whole body. If we scan every organ and joint, it’s nearly guaranteed we’ll find something, and perhaps many things. But not every finding needs treatment and most “abnormalities” will never cause problems.
So Who Should Consider Full Body MRI?
There are some cases where full body MRI screening may be appropriate:
People with genetic conditions that increase cancer risk (e.g., Li-Fraumeni syndrome, BRCA mutations)
Individuals with a strong family history of certain cancers
People in structured clinical trials evaluating MRI screening in high-risk groups
Are There Better Screening Tools?
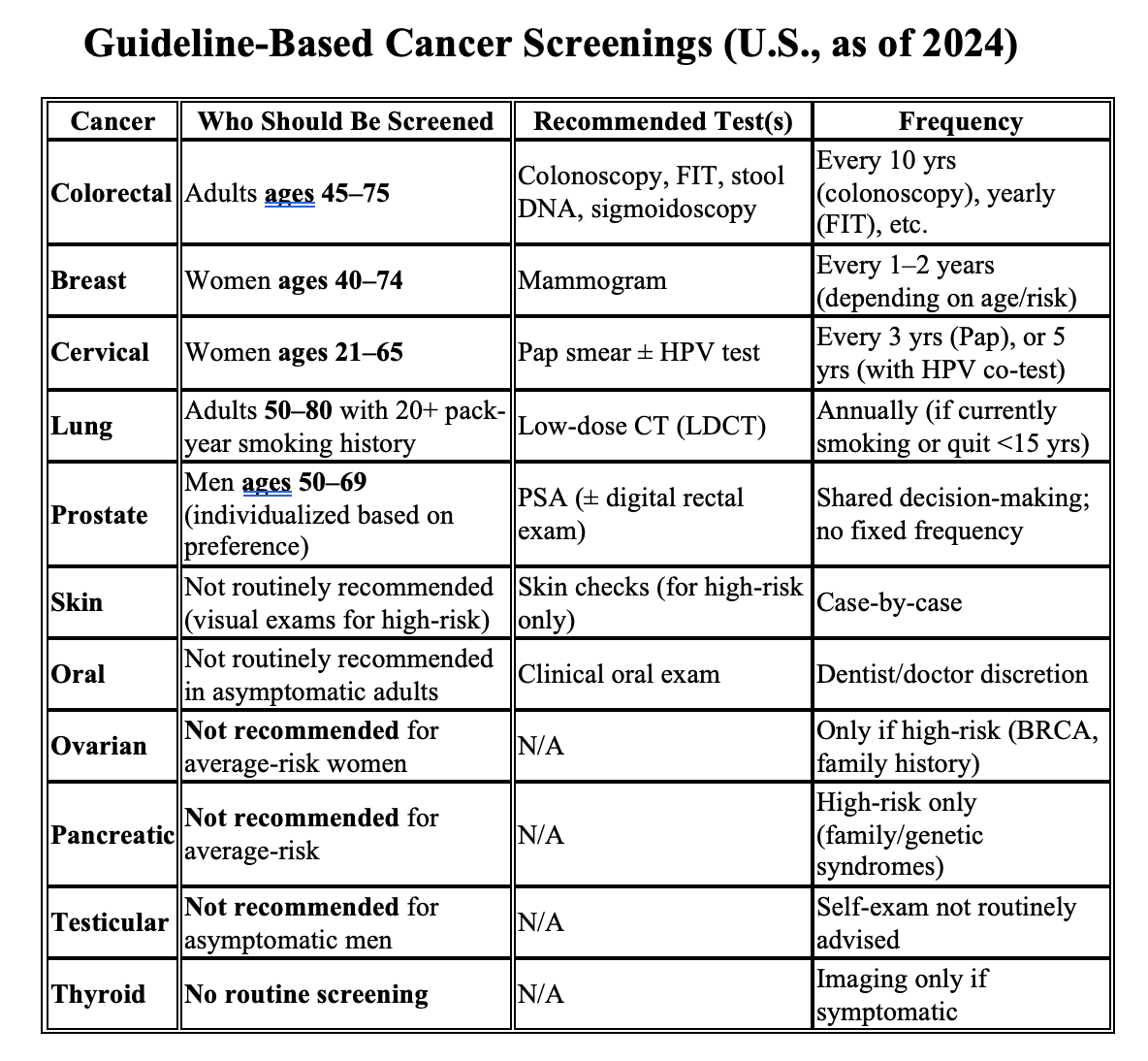
Yes—and they’re evidence-based. These include:
Mammograms for breast cancer
Colonoscopy for colon cancer
Pap smears and HPV testing for cervical cancer
Low-dose CT scans for lung cancer in long-term smokers
These tools are supported by years of research and population-level data. They also have defined follow-up plans based on risk factors. Here’s a summary table of general screening recommendations, which you should follow:
The TLDR
Full body MRI screening is not recommended for the average healthy person. The risks generally outweigh the benefits.
The chance of finding actual cancer is very low (<2%) in the average person.
It may lead to unnecessary tests, anxiety, and even harm from false positives.
If you’re at high risk for cancer based on family history or genetic factors, talk to your doctor about personalized screening options.
Proven preventative screening tests, such as pap smears, mammograms, and colonoscopies are the gold standard for cancer detection.
This perspective is widely supported by professional organizations across both specialty and preventive medicine, even if voices in the wellness space or on social media might suggest otherwise.
It’s completely understandable to want peace of mind about your health. But more testing isn’t always better. The best medical care is personalized, thoughtful, and based on evidence—not fear. Before pursuing a full body MRI, make sure to think through what you will do with the results and have a conversation with your doctor about your risk factors, concerns, and the best screening strategy for you.
If you’re enjoying these tips, please subscribe and comment. I’d love to hear what other topics you’d like to hear about. You can also connect with me on Instagram.
Rohit Jayakar, MD
About the Author: Rohit Jayakar MD specializes in non-surgical Sports Medicine (Physical Medicine & Rehabilitation). He treats a variety of musculoskeletal injuries, neurological injuries, and pain conditions.